
12,13 Accordingly, the primary objective of the International Nocturnal Oxygen (INOX) trial was to determine, in patients with COPD with nocturnal arterial oxygen desaturation who do not qualify for long-term oxygen therapy because of the absence of severe daytime hypoxemia, whether nocturnal oxygen provided for a period of 3 to 4 years affects mortality or the progression of COPD such that patients meet current specifications for long-term oxygen therapy. 12-14 Only two trials examined the effect of nocturnal oxygen on survival and progression to long-term oxygen therapy at 3 years of follow-up both trials had negative results but were underpowered, with only 38 patients undergoing randomization in one trial and 76 in the other trial. Three randomized trials directly addressed the issue of the effectiveness of nocturnal oxygen in patients not qualifying for long-term oxygen therapy who had desaturation overnight. 8,9 In addition, nocturnal oxygen desaturation in patients with COPD induces systemic inflammation that may also contribute to the pathogenesis of pulmonary hypertension and cardiovascular diseases. 5-7 This phenomenon is considered by many physicians as an indication for prescribing nocturnal oxygen because the progression of COPD to its end stages of severe hypoxemia, right heart failure, and death may result from the severity of desaturation occurring during sleep. 3,4 Alveolar hypoventilation (particularly during rapid-eye-movement sleep) and ventilation–perfusion mismatch are likely mechanisms. Sleep-related nonapneic oxygen desaturation often occurs in patients with COPD not qualifying for long-term oxygen therapy. 1,2 These two trials targeted patients with COPD with severe chronic daytime hypoxemia documented by arterial blood gas measurement. Two landmark trials that were published in the early 1980s provided evidence that, under very specific circumstances, long-term oxygen therapy used for at least 15 to 18 hours per day improves survival in patients with chronic obstructive pulmonary disease (COPD). (Funded by the Canadian Institutes of Health Research INOX number, NCT01044628.) Introduction Our underpowered trial provides no indication that nocturnal oxygen has a positive or negative effect on survival or progression to long-term oxygen therapy in patients with COPD. At 3 years of follow-up, 39.0% of the patients assigned to nocturnal oxygen (48 of 123) and 42.0% of those assigned to placebo (50 of 119) met the NOTT-defined criteria for long-term oxygen therapy or had died (difference, −3.0 percentage points 95% confidence interval, −15.1 to 9.1). Recruitment was stopped prematurely because of recruitment and retention difficulties after 243 patients, of a projected 600, had undergone randomization at 28 centers. The primary outcome was a composite of death from any cause or a requirement for long-term oxygen therapy as defined by the Nocturnal Oxygen Therapy Trial (NOTT) criteria in the intention-to-treat population. Patients with an oxygen saturation of less than 90% for at least 30% of the recording time on nocturnal oximetry were assigned, in a 1:1 ratio, to receive either nocturnal oxygen or ambient air from a sham concentrator (placebo). We designed this double-blind, placebo-controlled, randomized trial to determine, in patients with COPD who have nocturnal arterial oxygen desaturation without qualifying for long-term oxygen therapy, whether nocturnal oxygen provided for a period of 3 to 4 years would decrease mortality or the worsening of disease such that patients meet current specifications for long-term oxygen therapy. However, the efficacy of oxygen therapy for the management of isolated nocturnal hypoxemia is uncertain. Long-term oxygen therapy improves survival in patients with chronic obstructive pulmonary disease (COPD) and chronic severe daytime hypoxemia.

The most trusted, influential source of new medical knowledge and clinical best practices in the world.
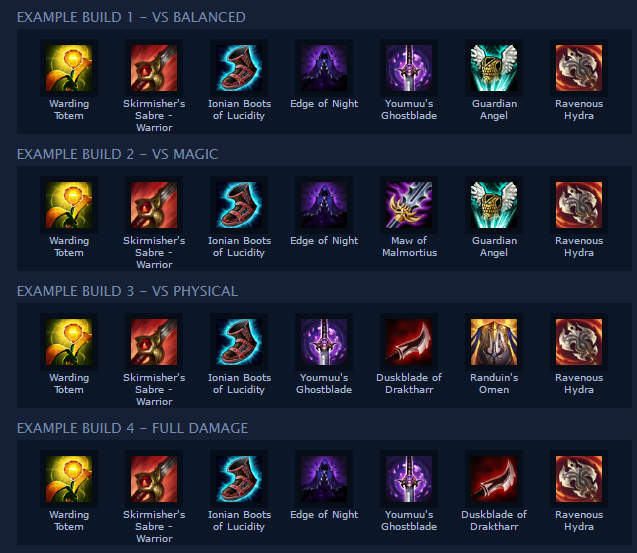
#Nocturn s7 license
Information and tools for librarians about site license offerings. Valuable tools for building a rewarding career in health care. The authorized source of trusted medical research and education for the Chinese-language medical community. The most advanced way to teach, practice, and assess clinical reasoning skills. Information, resources, and support needed to approach rotations - and life as a resident. The most effective and engaging way for clinicians to learn, improve their practice, and prepare for board exams. NEW! Peer-reviewed journal featuring in-depth articles to accelerate the transformation of health care delivery.Ĭoncise summaries and expert physician commentary that busy clinicians need to enhance patient care. NEW! A digital journal for innovative original research and fresh, bold ideas in clinical trial design and clinical decision-making.


 0 kommentar(er)
0 kommentar(er)
